Frozen shoulder aka adhesive capsulitis is a condition where your shoulder becomes stiff and very painful. The range of motion of your shoulder reduces, it can even become completely frozen. This happens due to adhesions forming within your shoulder capsule. The shoulder capsule resembles a sac-like structure that forms a sleeve around your shoulder joint. Untreated, frozen shoulder can take 2-3 years to resolve. Many treatments are available to reduce pain and improve range of motion, however recovery can still take many months.
Who gets frozen shoulder
A large, UK based study found that frozen shoulder affects 8.2% of men and 10.1% of women [1]. The peak age for developing symptoms is 56 years [2], and it is rare to develop this condition under the age of 40. Being diabetic, having thyroid issues and being overweight all increase your risk of developing a frozen shoulder [3]. Recent shoulder trauma or surgery, along with having had frozen shoulder on one side before, are also risk factors for this condition.

Causes
The exact cause of frozen shoulder is still not understood. We know that scar tissue forms within the shoulder capsule [4]. This scar tissue results in thickening and contracture of the joint capsule, essentially it shrinks and becomes stuck to itself. This is what limits the movement of the shoulder. Inflammation within the shoulder capsule is likely a major factor. As trauma, recent shoulder surgery and even vaccinations injected into the area [5] can increase your chances of being affected.
Symptoms
Frozen shoulder is characterised by an insidious onset, a progressive increase in pain, and gradual loss of motion [6]. Most people are relatively comfortable with the arm at the side, but often describe a sudden and excruciating pain when abrupt or end-range movements are attempted. Significant night pain is always present and often the reason people seek treatment.
Symptoms interfere with everyday activities such as driving, dressing and washing. Pain can extend from the neck, across the shoulder and down the arm on the affected side. There is normally a dull, constant throbbing pain, with severe sharp pain on movement [7]. Symptoms typically have three phases, each of these phases normally last 4-6 months on average [8] but each can last over 12 months.
- Phase one “freezing”: The first symptom is shoulder pain, followed by stiffness and gradual reduction in range of motion. The pain is typically worse at night, and aggravated when lying on the affected side. During this phase pain and stiffness will slowly build. This is the most painful phase and once completed, pain will reduce.
- Phase two “frozen”: Pain gradually eases but stiffness and limited range of motion remain. The muscles around the shoulder may become smaller and weaker as they are not being used.
- Phase three “thawing”: Pain completely goes as the stiffness gradually reduces and movement begins to return to normal, or near normal.

Treatments
The aim of treatment is to ease pain, reduce stiffness and to keep as much range of motion in the shoulder as possible whilst waiting for the condition to resolve. There are no cures, but the amount of movement available and the duration of the condition can be dramatically improved.
- Medication: anti-inflammatory such as ibuprofen, diclofenac and naproxen. or painkillers such as paracetamol and codeine are commonly prescribed by your GP. The problem here is the side effects associated with these medications and the long-term nature of frozen shoulder.
- Steroid injection: An injection into the shoulder capsule can provide good pain relief. The corticosteroids reduce inflammation and pain, but it dose not cure the condition, and symptoms tend to return. Many people do however welcome the relief that a steroid injection can bring, the benefit of which can last up to 24 weeks [9].
- Nerve blocks: This often involves multiple injection to block the nerves that send pain messages from the shoulder. Like the steroid injection, it often helps temporally , but it is not a cure.
- Hydrodistension: Another method of injecting into the shoulder joint, this time a procedure where the joint space is expanded by injecting a liquid i.e. saline mixed with a steroid. Also not a cure but combine with exercise therapy has been shown to give good result for as long as 6 months [10].
- Manipulation under anaesthetic This is a procedure where the shoulder is manipulated by the surgeon while you are under anaesthetic. However this is quite traumatic and has been shown to be no more effective than exercise alone [11].
- Arthroscopic capsular release. This is a form of keyhole surgery often done as a day-case procedure, it allows the surgeon to release the tight capsule. It has been shown to reduce pain and increase range of motion, and more effective than hydrodistension [12].
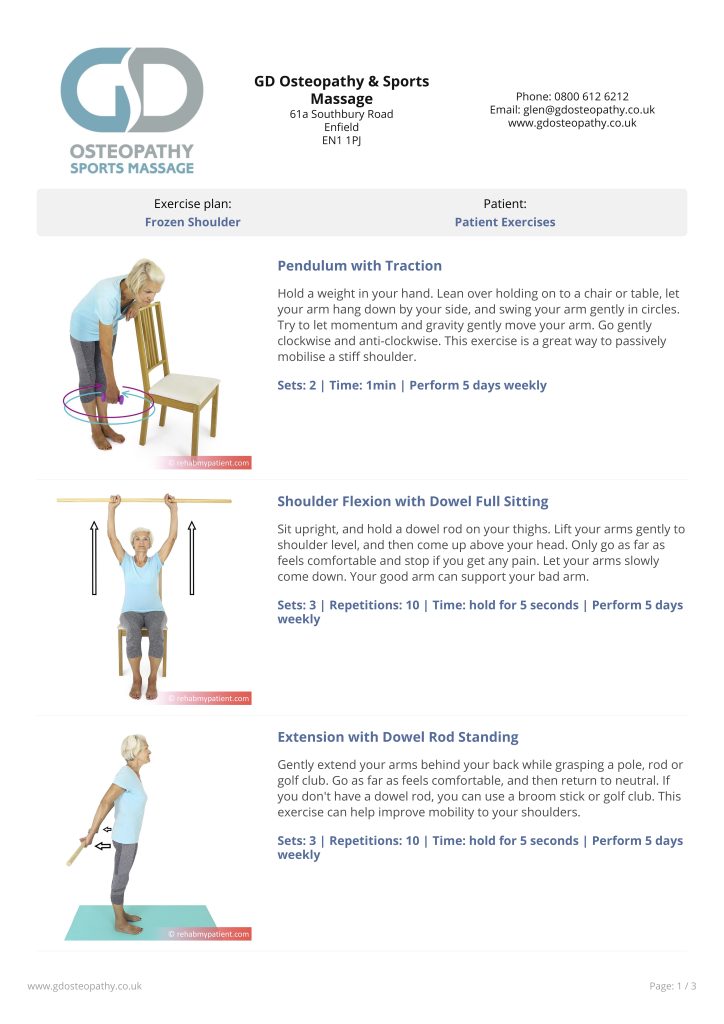
- Rehabilitation exercises: The aim of these exercises is to reduce stiffness and keep as full as possible range of motion. For most benefit, it is important to do the exercises regularly and not to push through pain. Many studies show the benefits of exercise in both maintaining and improving shoulder mobility [13]. See our frozen shoulder exercise plan.
- Manual therapy i.e. Osteopathy: This will include a full assessment of your shoulder and you’ll be provided with expert advice and treatment that is specific to your stage of injury. Manual therapy along side appropriate exercise, has been shown to improve both short and long-term benefits in pain level and range of motion [14]. For more information and advice contact the Enfield Osteopath.
References
- 1 Walker-Bone, K., Palmer, K., Reading, I., Linaker, C., Byng, T., Coggon, D., & Cooper, C. (2016). THE PREVALENCE AND IMPACT OF SOFT TISSUE MUSCULOSKELETAL DISORDERS OF THE NECK AND UPPER LIMB IN THE GENERAL POPULATION. RHEUMATOLOGY, 41, 36–36.
- Rizk, T. E., & Pinals, R. S. (1982, May). Frozen shoulder. In Seminars in arthritis and rheumatism (Vol. 11, No. 4, pp. 440-452). WB Saunders.
- Li, W., Lu, N., Xu, H., Wang, H., & Huang, J. (2015). Case control study of risk factors for frozen shoulder in C hina. International Journal of Rheumatic Diseases, 18(5), 508-513.
- Bunker T. D. (1997). Frozen shoulder: unravelling the enigma. Annals of the Royal College of Surgeons of England, 79(3), 210–213.
- Sahu, D., & Shetty, G. (2022). Frozen shoulder after COVID-19 vaccination. JSES international.
- Kelley, M. J., Mcclure, P. W., & Leggin, B. G. (2009). Frozen shoulder: evidence and a proposed model guiding rehabilitation. Journal of orthopaedic & sports physical therapy, 39(2), 135-148.
- Funk, L. (2016). Shoulder: The Articular Structures. ABC of Common Soft Tissue Disorders, 33.
- Schultheis, A., Reichwein, F., & Nebelung, W. (2008). Frozen shoulder. Diagnosis and therapy. Der Orthopade, 37(11), 1065-6.
- Sun, Y., Zhang, P., Liu, S., Li, H., Jiang, J., Chen, S., & Chen, J. (2017). Intra-articular steroid injection for frozen shoulder: a systematic review and meta-analysis of randomized controlled trials with trial sequential analysis. The American journal of sports medicine, 45(9), 2171-2179.
- Bryant, M., Gough, A., Selfe, J., Richards, J., & Burgess, E. (2017). The effectiveness of ultrasound guided hydrodistension and physiotherapy in the treatment of frozen shoulder/adhesive capsulitis in primary care: a single centre service evaluation. Shoulder & elbow, 9(4), 292-298.
- Wong, P. L. K., & Tan, H. C. A. (2010). A review on frozen shoulder. Singapore medical journal, 51(9), 694.
- Gallacher, S., Beazley, J. C., Evans, J., Anaspure, R., Silver, D., Redfern, A., … & Smith, C. (2018). A randomized controlled trial of arthroscopic capsular release versus hydrodilatation in the treatment of primary frozen shoulder. Journal of Shoulder and Elbow Surgery, 27(8), 1401-1406.
- Cho, C. H., Bae, K. C., & Kim, D. H. (2019). Treatment strategy for frozen shoulder. Clinics in orthopedic surgery, 11(3), 249-257.
- Dueñas, L., Balasch-Bernat, M., Aguilar-Rodríguez, M., Struyf, F., Meeus, M., & Lluch, E. (2019). A manual therapy and home stretching program in patients with primary frozen shoulder contracture syndrome: A case series. journal of orthopaedic & sports physical therapy, 49(3), 192-201.

